
Assessment – Sleep History
History includes:
- Difficulty initiating sleep or maintaining sleep (DIMS)
- Daytime function
- Habits before bedtime - sleep hygiene (relating to environmental factors, physiologic factors, behaviour and habits
- Onset of sleep problems
- Course/trajectory, frequency of insomnia symptoms (triggers, alleviators)
- Use of over the counter items such as products rich in caffeine (e.g. energy drinks, cola, coffee), weight loss supplements with guarana or prescribed products (e.g. Duromine)
- Medication use for sleep and other health issues (insomnia as medication side-effect?)
- Previous treatments used and effectiveness of these treatments
- Co-morbid conditions including excluding other potential causes of insomnia (mental health screening tools e.g. DASS 21, K10, Oestrogen Deficiency Score, or bloods e.g. TFTs, FSH if indicated)
Assess motivation to engage in behavioural therapy for insomnia – takes time and effort, but benefits persist over the long-term.
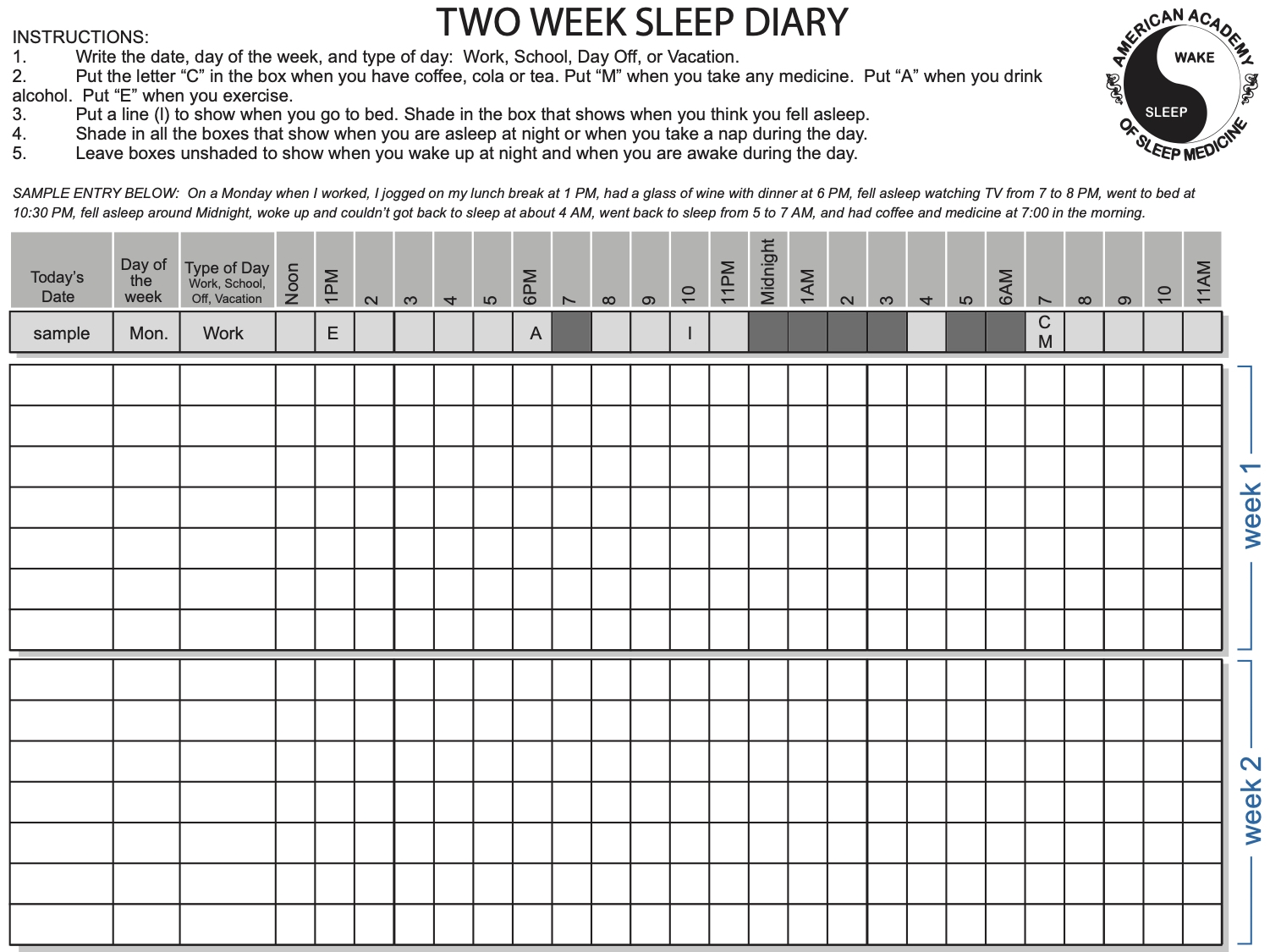
A sleep-wake or sleep diary (digital or paper based) should be used during the assessment and follow-up process of insomnia disorder.
A sleep diary:
Provides valuable information for the clinician to diagnose and guide treatment
Allows patients to:
i. Self-report their nightly sleep quality
ii. Self-report times spent asleep and awake
iii. Self-report activities assisting or hindering sleep
iv. Monitor their sleep habits
- Should be filled out in the morning as soon as possible after waking up
- Should be completed without ‘watching the clock’ throughout the night to note-down specific times
Table. Sleep diary data calculations
|

AHI - Apnoea-Hypopnoea Index
BBTi - Brief Behavioural Therapy for Insomnia
BMI - Body Mass Index (kg/m2)
BQ - Berlin Questionnaire
CBTi - Cognitive Behavioural Therapy for Insomnia
CELL - Coblation Endoscopic Lingual Lightening
COPD - Chronic Obstructive Pulmonary Disease
CVA - Cerebrovascular Accident
CPAP - Continuous Positive Airway Pressure
CSA - Central Sleep Apnoea
DASS - Depression Anxiety Stress Scale
DBAS - Dysfunctional Beliefs and Attitudes about Sleep
DBP - Diastolic Blood Pressure
DIMS - Difficulties Initiating and/or Maintaining Sleep
DISE - Drug-Induced Sleep Endoscopy
DISS - Daytime Insomnia Symptom Scale
ENT - Ear Nose and Throat
ESS - Epworth Sleepiness Scale
FOSQ - Functional Outcomes of Sleep Questionnaire
FSH - Follicle-Stimulating Hormone
FTP - Friedman Tong Position
GP - General Practitioner
HANDI - RACGP Handbook of Non-Drug Interventions
HGNS - Hypoglossal Herve Htimulation
ISI - Insomnia Severity Index
K10 - Kessler Psychological Distress Scale
MAD - Mandibular Advancement Device
MAS - Mandibular Advancement Rplint
MBS - Medicare Benefits Schedule
MMA - Maxillomandibular Advancement Surgery
MRA - Mandibular Repositioning Appliance
ODI - Oxygenation Desaturation Index
OSA - Obstructive Sleep Apnoea
PLMD - Periodic Limb Movement Disorder
PT - Positional Therapy
PTSD - Post-Traumatic Stress Disorder
PSG - Polysomnography
QSQ - Quebec Sleep Questionnaire
REM - Rapid Eye Movement
RFTB - Radiofrequency Thermotherapy of the Tongue Base
SBP - Systolic Blood Pressure
SCI - Sleep Condition Indicator
SE - Sleep Efficiency
SF36 - Short-Form (36) Health Survey
SMILE - Submucosal Minimally Invasive Lingual Excision
SNRIs - Serotonin-Norepinephrine Reuptake Inhibitors
SOL - Sleep Onset Latency
SSRI - Selective Serotonin Reuptake Inhibitors
TFTs - Thyroid Function Tests
TIB - Time In Bed
TORS - Transoral Robotic Surgery
TST - Total Sleep Time
UPPP - Uvulopalatopharyngoplasty
WASO - Wake After Sleep Onset